Two RCCA Oncologists Explain How Radiopharmaceuticals Are Transforming Advanced Prostate Cancer Care
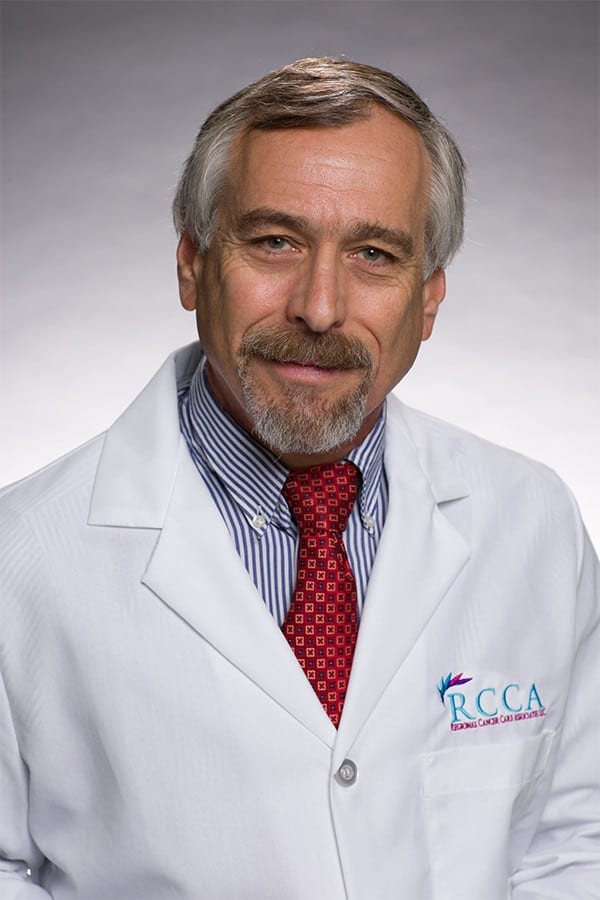
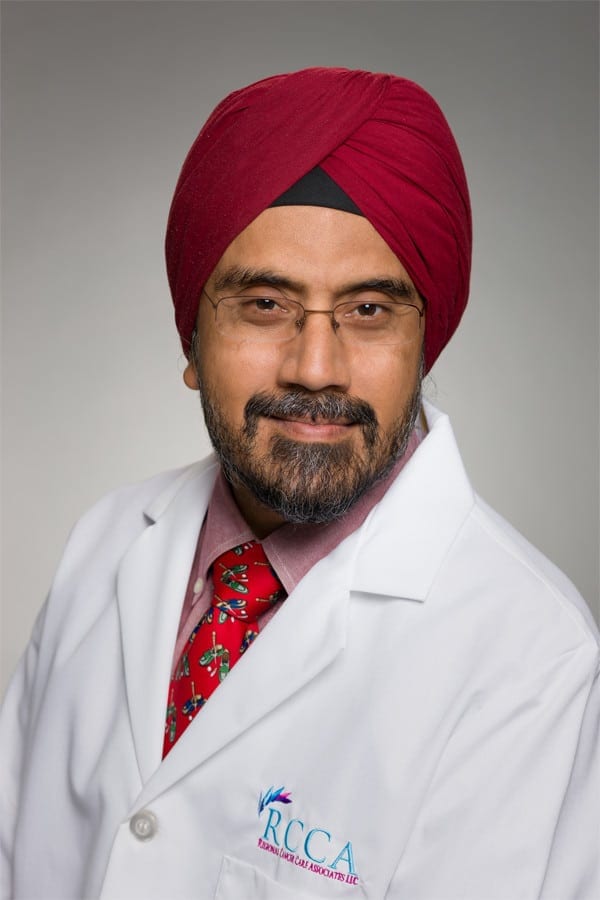
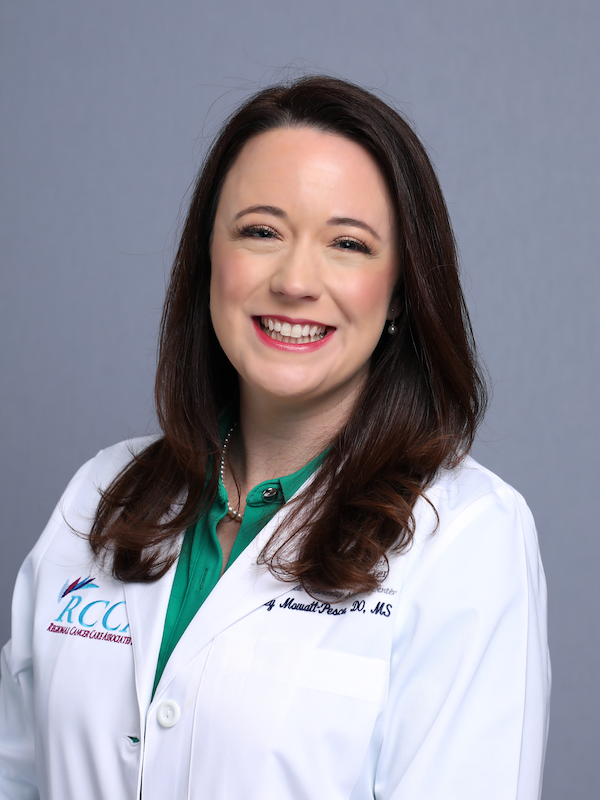
An innovative approach to administering radiation therapy via infusion is helping patients with advanced prostate cancer live longer while maintaining their quality of life, say two