
PSMA Therapy for Metastatic Prostate Cancer
A targeted, infused therapy that delivers radiation directly to cancerous cells has been shown to extend survival in many patients with metastatic prostate cancer. The
HIPAA Alert: Potential Data Breach Learn More
Questions on Oncology, Hematology and/or Infusion Clinical Services due to COVID-19 Crisis – CALL 833-698-1623
Important Information for Our Patients Regarding the Coronavirus.
RCCA Providing Area Cancer Patients with Access to Care During Coronavirus Outbreak
RCCA Offering Patients Virtual Visits During Coronavirus Pandemic
“You look kind of yellow.”
It was not the sort of dinner table conversation Brenda Morgart had anticipated when she and her husband got together with her niece and the niece’s boyfriend for a meal one night in October 2020. Nor could she have anticipated the life-changing events that would follow from her niece’s observation.
That chain of events began when Ms. Morgart looked in the mirror and saw that her skin did, indeed, have a yellow cast. That prompted a trip to an urgent care center, where a physician noted that the Franklin, NJ resident’s eyes were also yellow. The doctor diagnosed jaundice and sent her straight to the emergency room.
Following initial evaluation in the ER, Ms. Morgart underwent a procedure called endoscopic retrograde cholangiopancreatography, or ERCP. The procedure combines X-ray imaging and insertion of a long, flexible lighted scope into the abdomen to assess the liver, bile ducts, gall bladder and pancreas. The gastroenterologist performing the ERCP found a blockage in one of the bile ducts – thin tubes that connect the liver to the small intestine – and placed a stent in the duct to relieve the blockage.
While the blockage and need for an ERCP procedure obviously were unwelcome, they didn’t entirely surprise Ms. Morgart because she previously had been diagnosed with primary biliary cholangitis, an autoimmune disease in which the bile ducts are slowly destroyed. “I wasn’t thinking about cancer,” she says of her mindset at the time.
The first ERCP was followed by three others in the weeks ahead, including one to place a larger stent, and one to re-evaluate her condition after she developed pancreatitis. In December 2020, a gastroenterologist in Morristown performed a more-sophisticated procedure known as ERCP with SpyglassTM, in which the bile ducts can be visualized by means of a 6,000-pixel fiber-optic probe attached to a tiny camera. What the gastroenterologist found with the SpyglassTM prompted Ms. Morgart to see the next of many doctors who would be involved in her care – a surgeon at Morristown Medical Center.
A frightening diagnosis – and a major surgery
“Let’s talk about how we’re going to get this cancer out of you,” the surgeon told her at their first meeting, explaining that she had pancreatic cancer. That news, while devastating for anybody, was all the more upsetting because Ms. Morgart had a friend, a nurse, who had died of the disease just a few years before. After delivering the diagnosis, the surgeon went on to explain that Ms. Morgart was among the minority of people with pancreatic cancer who are candidates for a Whipple procedure, a major, complex surgery that involves removal of the head of the pancreas, a portion of the small intestine, a portion of the stomach and the bile duct.
Ms. Morgart underwent the multi-hour operation on December 29, 2020. Because of COVID-19 protocols, her husband could not be at the hospital when she was diagnosed or as she went into surgery; nor could he visit her during her postoperative stay. Ms. Morgart did have visitors, however: oncologists from the Morristown area. When the time came to discuss treatment, Ms. Morgart chose Jumana Chatiwala, MD, and May Abdo-Matkiwsky, DO, whom she met at Newton Medical Center at the beginning of her journey. Board-certified medical oncologists practicing in the Sparta, NJ offices of Regional Cancer Care Associates (RCCA) – one of the nation’s largest networks of oncology specialists — Dr. Chatiwala and Dr. Abdo-Matkiwsky talked with her about plans for her subsequent treatment.
“They got all of the cancer at surgery,” Ms. Morgart explains, but with a diagnosis of Stage 3 pancreatic cancer, indicating spread to the lymph nodes, preventative chemotherapy was indicated to reduce the risk of recurrence.
Getting through chemo with the help of a caring team
Ms. Morgart began her 12-cycle course of chemotherapy early in the new year – and had a rough go of it right from the start. “I got very sick after the first dose, and had a neurologic side effect after the second,” she recalls, adding that she seriously considered stopping treatment.
She says her decision – and ability – to go on and complete the full course of chemotherapy was due in large measure to the care she received from the medical oncologists, nurses, and other staff at RCCA’s Sparta office.
“They were always on top of everything going on,” Ms. Morgart says, noting that Dr. Chatiwala, who took the lead in providing her care, and nurse Lori Winters, RN, offered encouragement and compassionate support as well as carefully adjusting the chemotherapy regimen as needed and taking several steps to ease the side effects of treatment.
“Everybody in the office was phenomenal,” she says, adding that the convenience of receiving her chemotherapy infusions and related care 12 minutes from her house was a major advantage during her treatment. Ms. Morgart says, “My boss was trying to push me to go up to Yale, where he knew someone, but I said no,” because of her confidence in the care she was receiving from Dr. Chatiwala and the RCCA team.
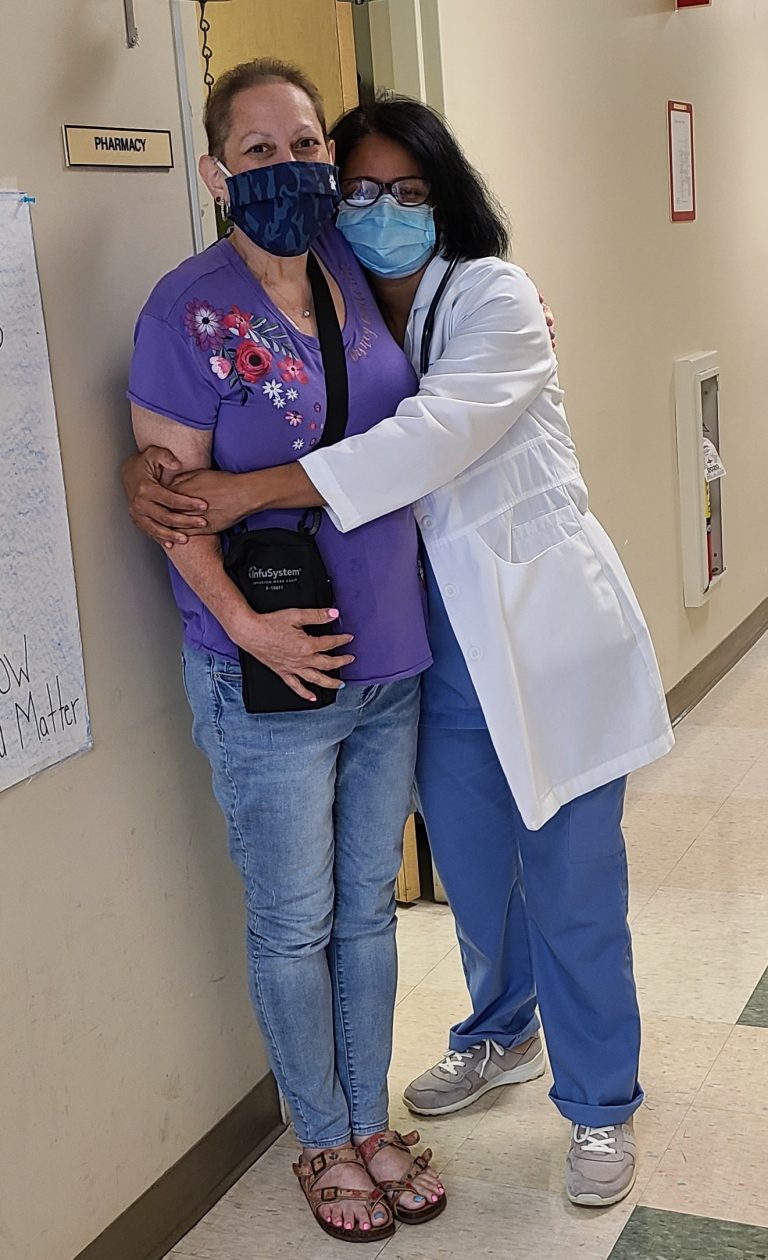
Ms. Morgart completed her chemotherapy in July 2021. When she rang the bell in the Sparta office to mark her last treatment, Dr. Chatiwala was there to give her a hug. “She’s such a good person,” Ms. Morgart says of the physician, who has practiced in RCCA’s Sparta care center for more than six years. “She’s phenomenal. She was always there. She would come in and hold my hand,” during chemotherapy infusions, she adds of Dr. Chatiwala.
A survivor’s advice to others fighting cancer
At the start of 2022, a little more than a year after her Whipple procedure and six months after completing chemotherapy, Ms. Morgart was doing well but “not 100% back to normal” in terms of her energy level.
Looking back on her experience from the vantage point of a new year, Ms. Morgart says that an attitude and an approach helped her throughout her treatment.
“I’ve always been an ‘It is what it is, just deal with it’ person,” she explains, adding that she focused her energy on what needed to be done rather than on the “Why me?” question.
Turning to the approach that sustained her, Ms. Morgart says, “You have to be honest with yourself and all of your doctors and care team about what you’re feeling and going through.” She emphasizes, “If you’re scared, tell them that, too,” explaining that when she began to experience significant anxiety before chemotherapy sessions, she talked with Dr. Chatiwala, who prescribed a mild anti-anxiety medication that helped calm her and make the treatment more tolerable.
Dr. Chatiwala heartily echoes her patient’s advice. “There is so much that we can do today for people with cancer. That includes the major advances in treatment, such as the immunotherapies, latest chemotherapy regimens, and other cutting-edge therapies and clinical trials that RCCA makes available in community settings such as our Sparta office. But it also includes a wealth of supportive treatments and approaches to avoid or minimize side effects and to enhance patients’ quality of life during treatment. Open, honest communication between the patient and clinical team is key to all aspects of care, but it is particularly important in helping patients deal with their very understandable worries and concerns.”
The medical oncologist adds, “Brenda epitomizes the patient who is committed to being a full partner in her treatment. It is an honor for us to care for her – and for all of our patients. While people are very appreciative of what we do for them, I don’t know that they can always appreciate how much we are inspired by their courage and their resilience.”
With two grandchildren and a “terrier mutt” named Delilah who arrived just before she began chemotherapy, Ms. Morgart is looking to the future while grateful for the doctors and others who helped her through an incredibly trying year. “Rely on your care team and their support, and be totally honest with them,” she reiterates for others in the midst of their own battles with cancer.
*******
After earning her medical degree from Maharaja Sayajirao University in India, Dr. Chatiwala completed her residency in internal medicine and fellowship in hematology-oncology at St. Joseph’s Regional Medical Center in Paterson, NJ. She is board-certified in internal medicine, hematology, and medical oncology, and is a member of the American Medical Association, American Society of Clinical Oncology, and American Society of Hematology. She has been honored as a Jersey’s Best magazine “Top Doctor” over several years.
Dr. Chatiwala is among the 90+ cancer specialists who treat patients at 25 RCCA care centers located throughout New Jersey, Connecticut, Maryland, and the Washington, DC, area. RCCA oncologists and hematologists see more than 23,000 new patients each year and provide care to more than 225,000 established patients, collaborating closely with their patients’ other physicians. They offer patients the latest in cutting-edge treatments, including immunotherapies and targeted therapy, as well as access to a wide range of clinical trials. In addition to serving patients who have solid tumors, blood-based cancers, and benign blood disorders such as anemia, RCCA care centers also provide infusion services to people with a number of non-oncologic conditions—including multiple sclerosis, Crohn’s disease, asthma, and rheumatoid arthritis—who take intravenously-administered medications.
To learn more about RCCA, call 1-844-346-7222 or visit RCCA.com.
For more information or to schedule an appointment,
call 844-346-7222. You can also schedule an appointment by calling the RCCA location nearest you.

A targeted, infused therapy that delivers radiation directly to cancerous cells has been shown to extend survival in many patients with metastatic prostate cancer. The

Patients receiving treatment from Regional Cancer Care Associates in Moorestown are in good hands. Five of its physicians — Dr. Seth Berk, Dr. Maurice Cairoli, Dr.

The world of cancer treatment is rapidly evolving. New therapies are being discovered, and existing ones have improved, resulting in better patient outcomes. Regional Cancer

Regional Cancer Care Associates is one of fewer than 200 medical practices in the country selected to participate in the Oncology Care Model (OCM); a recent Medicare initiative aimed at improving care coordination and access to and quality of care for Medicare beneficiaries undergoing chemotherapy treatment.