
2026 Cancer Statistics
Cancer Death and Diagnosis Statistics for 2026: 2 RCCA Oncologists Provide Insights into the Numbers The latest statistics from the American Cancer Society (ACS) detail
HIPAA Alert: Potential Data Breach Learn More
Questions on Oncology, Hematology and/or Infusion Clinical Services due to COVID-19 Crisis – CALL 833-698-1623
Important Information for Our Patients Regarding the Coronavirus.
RCCA Providing Area Cancer Patients with Access to Care During Coronavirus Outbreak
RCCA Offering Patients Virtual Visits During Coronavirus Pandemic
Lymphoma can be a difficult disease for the average person to understand. It occurs in the lymphatic system, which is not nearly as well known to most people as, say, the digestive system or nervous system. And, unlike colon cancer or breast cancer, it can begin anywhere in the body rather than in a specific organ. Further, there are numerous types of lymphoma, although they generally can be classified as either Hodgkin lymphoma (HL) or non-Hodgkin lymphoma (NHL). However, that distinction can create uncertainties of its own, with people asking, in a manner reminiscent of a frequent question about basal cell vs. squamous cell skin cancers, “Which is the worse of the two?”
Regional Cancer Care Associates (RCCA) is one of the nation’s largest cancer care networks, providing care at more than 20 locations near you in New Jersey, Connecticut, Massachusetts, and the Washington, D.C., area. Here, two board-certified hematologists/medical oncologists with RCCA provide an overview of lymphoma, discuss common presenting symptoms and risk factors for the cancer, and outline treatment approaches for the most common form of the disease.
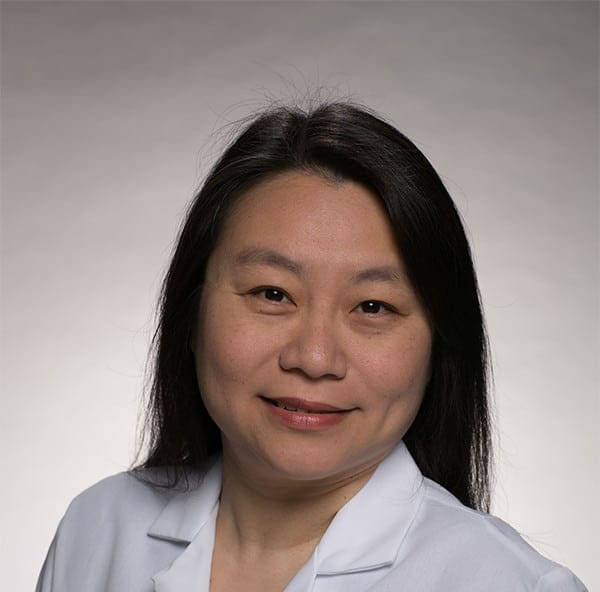
“Lymphomas are cancers that begin in the lymphatic system, which also is known as the lymphoid system,” explains Aileen L. Chen, MD, who practices at RCCA’s Freehold and Holmdel, NJ, offices. Dr. Chen adds, “Much like the circulatory system that carries blood throughout the body, the lymphatic system is an extensive network of vessels and organs. It collects excess fluid – lymph – from different tissues, filters out harmful substances and waste, and then returns the fluid to the blood stream.” She adds, “The lymphatic system is a component of the body’s immune system and is home to many infection-fighting white blood cells, called lymphocytes. This is why swollen lymph nodes can be a sign of infections or of cancers of the white blood cells, such as leukemia and lymphoma.”
Victor Aviles, MD, who practices with RCCA at Hematology and Oncology Specialists of Cape Code in North Falmouth, MA, adds, “Swollen lymph nodes in the neck, armpit, or groin are among the most common presenting features of lymphoma. However, these masses, which typically have a rubbery or firm texture, can be caused by many conditions other than cancer, so they are not reason to panic, but they definitely are reason to see your primary care physician without delay. Meanwhile, a less common form of the disease known as cutaneous lymphoma can be marked by red scaly patches or red or purple lumps on the skin. Again, many common, non-cancerous dermatologic conditions can cause similar symptoms, which is why a prompt visit to the dermatologist is in order when you note any new or unusual changes to your skin.” Dr. Aviles adds that other common symptoms of lymphoma, including fatigue, fever, and night sweats, also can represent any number of conditions. He explains that in assessing a patient who presents with these symptoms, a primary care physician will perform a thorough examination, take a detailed history to look for risk factors and an overall pattern that would suggest lymphoma rather than other causes, and order a complete blood count and other blood tests.
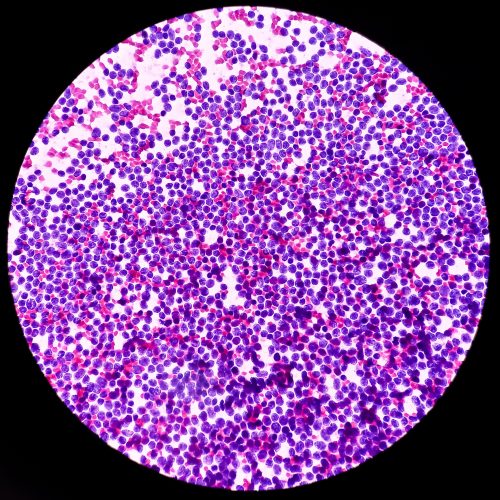
“Depending on the findings of that initial workup, the patient may be referred for a lymph node biopsy,” Dr. Aviles says. He explains that a pathologist’s identification of cancerous cells in lymph tissue obtained from the biopsy is key to the definitive diagnosis of lymphoma. Imaging studies also may be ordered to assess the lymph nodes and to look for signs that lymphoma has spread to other organs, while bone marrow biopsy and genetic testing also may be ordered following a diagnosis of the disease.
Dr. Chen says, “Lymphoma can occur at any age, but it is more common in people who are 60 years and older. It also is somewhat more common in men than women and in white people versus people from other racial groups. Certain infections, including human immunodeficiency virus, or HIV, can increase the risk for developing lymphoma, as can prior radiation therapy or chemotherapy, exposure to pesticides, some autoimmune disorders, and a family history of the disease.” [American Cancer Society, Non-Hodgkin Lymphoma Risk Factors]
Dr. Chen adds, “There are dozens of types of lymphoma, but we typically categorize those conditions as being either Hodgkin lymphoma or non-Hodgkin lymphoma. Of the two, NHL includes far more forms of the disease and is more common. The American Cancer Society estimates than approximately 80,350 people in the United States will be diagnosed with NHL this year, as compared to roughly 8,720 diagnoses of HL.” [ACS, Key Statistics for Non-Hodgkin Lymphoma; Key Statistics for Hodgkin Lymphoma]
The hematologist/medical oncologist adds that the main difference between the two forms of lymphoma is the type of cells affected. “Hodgkin Lymphoma is characterized by the presence of Reed-Sternberg cells, which are large, abnormal lymphocytes. By contrast, in NHL, other types of immune cells, including B cells, T cells, and so-called natural killer cells are affected.”

Dr. Chen says that while non-Hodgkin lymphoma tends to be more aggressive than HL, recent years have seen an intense research focus on the disease, resulting in the development of a wide range of therapies. “We have more options than ever to treat the various forms of NHL, such as diffuse large B-cell lymphoma, follicular lymphoma, and T- cell lymphomas. This enables us to develop highly individualized treatment plans that draw on various therapies and combinations and sequences of therapies to tailor treatment to a patient’s specific situation and offer him or her the best outcomes possible,” she says. Dr. Chen adds that options for treating NHL include immunotherapy, targeted therapy, chemotherapy, and radiation therapy. “Several factors help shape our choice of therapeutic regimen, including whether the lymphoma is aggressive or slow-moving, the stage at which it is diagnosed, and the patient’s overall health and treatment preferences,” the cancer specialist says.
Dr. Aviles notes that the rate of new cases of NHL has declined by about 1% each year over the last 10 years, while the death rate fell by roughly 2% annually from 2013 to 2022, the last year for which complete statistics are available. [American Cancer Society, Key Statistics for Non-Hodgkin Lymphoma] He says, “The reduced mortality that we’re seeing with NHL speaks to the effectiveness of the treatments that we have available to us today and that we’re able to deliver to people at community-based cancer centers, such as the offices of RCCA, close to their homes. However, there is still far more progress to be made. Just under 20,000 people in the United States will die from non-Hodgkin lymphoma this year, [American Cancer Society, Key Statistics for Non-Hodgkin Lymphoma] and while the 5-year survival rates for common forms of NHL are high – such as a 97% rate for follicular lymphoma – those rates decline considerably when lymphoma has spread throughout the body. [American Cancer Society, Survival Rates and Factors That Affect Prognosis (Outlook) for Non-Hodgkin Lymphoma] This underscores the importance of early diagnosis and treatment, and of seeing your physician promptly for evaluation of any concerning symptoms.”
********************************
Dr. Aviles and Dr. Chen are among roughly 100 medical oncologists and hematologists who practice with Regional Cancer Care Associates (RCCA), one of the nation’s largest networks of oncology specialists. RCCA has more than 20 locations near you across New Jersey, Connecticut, Massachusetts, and the Washington, D.C., area. RCCA’s cancer specialists see more than 30,000 new patients each year and provide care to more than 265,000 established patients, collaborating closely with those patients’ other physicians. RCCA physicians offer patients innovative therapies, including immunotherapies and targeted therapy, as well as access to approximately 300 clinical trials. In addition to serving patients who have solid tumors, blood-based cancers, and benign blood disorders, RCCA care centers also provide infusion services to people with a number of non-oncologic conditions—including multiple sclerosis, Crohn’s disease, asthma, iron-deficiency anemia, and rheumatoid arthritis—who take intravenously-administered medications.
To learn more about RCCA, call 844-346-7222 or contact RCCA today.
For more information or to schedule an appointment,
call 844-346-7222. You can also schedule an appointment by calling the RCCA location nearest you.

Cancer Death and Diagnosis Statistics for 2026: 2 RCCA Oncologists Provide Insights into the Numbers The latest statistics from the American Cancer Society (ACS) detail

If you’ve been diagnosed with breast cancer, you may have heard radiation therapy discussed as part of your treatment plan. This approach is commonly used

Cancer and its treatment often impact a person’s quality of life. In the case of prostate cancer, a man’s sex life may be affected. Sexual

Regional Cancer Care Associates is one of fewer than 200 medical practices in the country selected to participate in the Oncology Care Model (OCM); a recent Medicare initiative aimed at improving care coordination and access to and quality of care for Medicare beneficiaries undergoing chemotherapy treatment.